To better understand antibiotic resistance (AMR) in bacteria, agencies within USDA, the Food and Drug Administration (FDA), the Centers for Disease Control and Prevention (CDC), and other federal and state partners work collaboratively through the National Antimicrobial Resistance Monitoring System (NARMS). Recent ground-breaking scientific advances are helping NARMS partners to improve their understanding about how some disease-causing bacteria can become resistant to antibiotics.
NARMS monitors bacteria that include Salmonella, Campylobacter, E. coli and Enterococcus. For 20 years, NARMS researchers have grown such bacteria from cultures taken from humans, food animals and foods derived from animals. The results of monitoring these “isolated” bacteria are findings that are published in scientific publications and annual reports to inform professionals, scientists and the public, about bacterial AMR trends in the United States.
In traditional “phenotypic” testing, bacteria are grown in the presence of different concentrations of various antibiotics. Bacteria that do not grow in the presence of a test antibiotic are called ‘susceptible’ and those that do grow are called ‘resistant.’
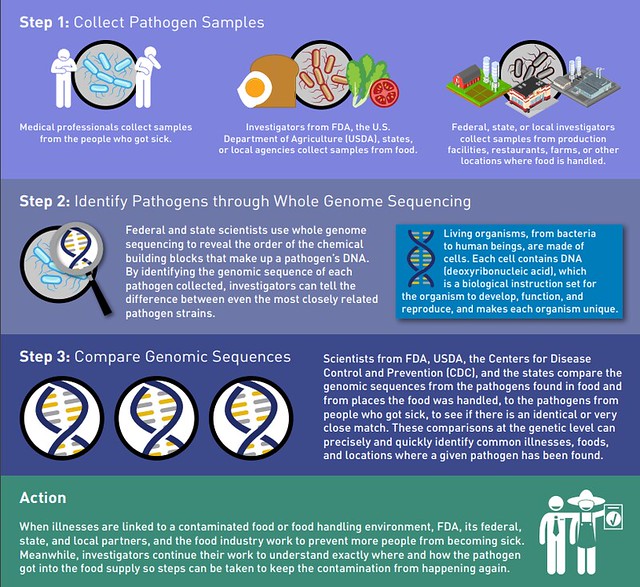
Today, however, the same information can be generated through newer technology called ‘whole genome sequencing’ (WGS). Using this technology, researchers can observe how deoxyribonucleic acid (DNA) or genes in bacterial populations can be shared via plasmids or other mobile elements. AMR genes shared this way lead to ‘acquired resistance.’
What makes WGS ground-breaking is that it can help researchers predict AMR more efficiently, using a singular WGS workflow. Initial studies done by NARMS partners using WGS and phenotypic data indicate a high correlation between the presence of AMR genes and the phenotypic data.
Emerging tools such as metagenomics are focusing on applying sequencing to the sample itself, eliminating the need to isolate and sequence bacteria from the sample. By directly applying the sequencing technology to a test sample, we can reduce analytic time, increase the efficiency of the intended outcome (surveillance or therapy) and bring about significant cost savings. As a result, it won’t be surprising if the NARMS and other AMR programs in the U.S. and the world begin to rely only on WGS analysis in place of the phenotypic testing for some aspects of their surveillance programs.
Most of the bacteria currently isolated in the NARMS program have been subjected to WGS. Information generated by WGS can be readily analyzed for the presence of AMR genes and then uploaded into a public database hosted by the National Center for Biotechnology Information (NCBI) at NIH. From there, the public can access this information including the type of AMR genes present.
The WGS-based approach seems to offer valuable information to augment or supplant the phenotypic approaches. When it is coupled with the One Health approach, WGS will allow us to understand AMR at a deeper level and thus help increase the longevity and even efficacy of currently used antibiotics.
